Neuromodulation for pain
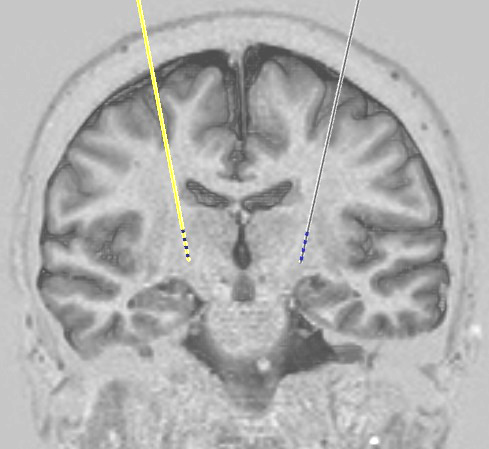
Neuromodulation means the use of implanted stimulator systems (a bit like heart pacemakers) that send small electrical pulses to specific parts of the nervous system. We treat several different types of pain this way, and the exact part of the nervous system that we choose to stimulate depends on the type of pain you have and where it is located in your body. Stimulators may for example be applied to the brain, spinal cord, or peripheral nerves.
These treatments involve surgery and therefore a degree of risk. It is important that all other treatment methods (including all appropriate medication) have been tried first, under the supervision of a pain specialist (i.e. a doctor working in a specialist pain clinic, or a neurologist if the problem is headache). Referrals to us should come from these specialists.
It is important to have realistic expectations of the benefits of treatment before it is undertaken. The aim of stimulation is to lessen pain, and in many cases pain cannot be got rid of completely. We have to be clear before treatment that even just a partial reduction in pain would be valuable, as an expectation of complete relief will often result in disappointment.
Some of the types of pain we treat, and the types of treatment used for them, are described below.
Headache and facial pain
Headache is a very common problem. In the vast majority of cases it can be effectively treated with painkilling medication, but a few people suffer with severe headaches that do not respond to the usual tablets or injections. In such cases neuromodulation may be useful.
Migraine
Migraine headache is one-sided, often throbbing, and may be accompanied by nausea/vomiting or sensitivity to light. Episodes last from hours up to a few days. Some people experience warning symptoms before the headache called an 'aura', for example seeing zigzag lines, temporarily losing part of the field of view, or having difficulty with speech. The frequency of attacks is variable but patients coming to us for treatment generally have 'chronic migraine' where headache is present more days than not.
Before considering neuromodulation patients would in general have tried preventative medication including beta blockers, topiramate, sodium valproate, pizotifen, amitriptyline, and gabapentin, and would usually also have tried Botox treatment.
Where none of these have been effective, occipital nerve stimulation may be appropriate.
Cluster headache
This is an extremely severe form of headache which affects mainly men. Attacks typically last 15 minutes to 3 hours and there may be multiple episodes per day. Pain is located in or around the eye or temple and affects only one side of the head, which for each patient is always the same side. It is accompanied by other symptoms including facial flushing, tearing, and running nose. Attacks usually come in clusters as the name suggests, with lengthy headache-free periods (months) between clusters. However by the time they reach us patients have typically developed 'chronic cluster headache' where attacks occur virtually every day.
Before considering neuromodulation patients would usually have tried preventative medications including verapamil, steroids, lithium, topiramate and gabapentin.
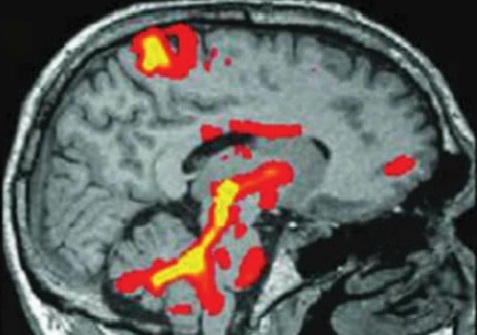
We would usually try occipital nerve stimulation initially. If this is unsuccessful, deep brain stimulation may be effective. Cluster headache uniquely responds to stimulation of an area of the brain called the posterior hypothalamus.
Trigeminal neuralgia and anaesthesia dolorosa
Trigeminal neuralgia (TGN) is a type of severe facial pain. It is almost always felt only on one side of the face, and may affect the jaw, cheek, forehead, or more than one of these areas. It comes in brief episodes that are classically described as "lancinating" which means a severe, stabbing pain. Often there will be a "trigger" that sets it off such as wind on the face or brushing the teeth.
Neuromodulation is not usually a first-line treatment for TGN. Medications such as carbamazepine are usually tried first. Surgery may also be an option; TGN is thought in most cases to result from a blood vessel compressing the trigeminal nerve near the brainstem, and an operation called microvascular decompression (MVD), where the vessel is moved off the nerve, is often very effective. In other cases we might recommend a procedure where an injection is given to part of the trigeminal nerve called the "ganglion", or a special needle is inserted into the same area to heat it up. Both the injection and the heating work by deliberately damaging the nerve to stop it carrying pain signals. Another treatment involves treating the nerve with highly focussed radiation using a machine called a Gamma knife.
Unfortunately a complication that can occur in a small percentage of people with any of the surgical methods of treatment, or with the Gamma knife, is "anaesthesia dolorosa", which is a situation where the face goes numb but is still extremely painful. When this happens, none of the treatments above is likely to work any more. In this situation, deep brain stimulation may be an option.
Back pain
Failed back surgery syndrome
This is a condition affecting people who have had back surgery, for example a laminectomy, and are left with chronic pain in the back and/or the legs. They have often had more than one operation and ironically surgery will usually have been done to address a pre-existing pain problem.
More back surgery, particularly in those who have already had more than one procedure, may not be effective. In general, the more operations a patient has had already, the less likely it is that another will help.
In this situation, spinal cord stimulation may be an option. This is often more effective for leg pain than back pain, and so has generally been regarded as most suitable for patients with either leg pain alone, or leg pain that is worse than their back pain. However we will consider each case on its own merits and we are presently running a clinical trial of spinal cord stimulation for people whose back pain is worse than their leg pain (the PROMISE trial). Patients who are suitable will be invited to take part in this study.
Spinal cord injury
Injury to the spinal cord can result in chronic severe pain in areas below the level of the injury (thus if the injury is at chest level, pain may affect the lower part of the trunk and the legs, while if the injury is to the neck, the upper trunk and arms may also be affected). The pain may be burning in nature or like severe pins and needles, and is often felt in areas that are otherwise numb.
Where pain-relieving medication fails, deep brain stimulation may be considered for this type of pain. However, as with post stroke pain (see below) it is important to note that this can be difficult when the pain is spread over extensive areas of the body, for example if the abdomen and both lower limbs are affected.
Abdominal pain
Visceral pain
The viscera are the internal organs, and sometimes the abdominal viscera can be a source of pain. One of these organs is the pancreas, and one condition that can cause chronic severe abdominal pain is pancreatitis. We have also seen cases of severe pain following bowel surgery.
Severe visceral pain that is unresponsive to other treatments can sometimes be treated using spinal cord stimulation.
Post hernia surgery pain
Inguinal (groin) hernias are a common problem and often require an operation to repair them. Whilst the surgery is straightforward and usually successful, some people after surgery can experience chronic pain in the groin.
When this 'post herniorrhaphy pain' is severe and does not respond to other painkilling methods, it may be treated using peripheral nerve stimulation or dorsal root ganglion stimulation.
Limb pain
Phantom pain
Most people who have lost part or all of an arm or leg will experience some form of "phantom" sensations, which are sensations that feel like they are in the missing limb. Commonly these sensations are painful, and sometimes severely so. The precise cause of phantom limb pain is unclear. It may include abnormal pain signals coming from cut nerve ends in the amputation stump, but it is also likely that the part of the brain that used to receive signals through those nerves is malfunctioning because it no longer has any normal sensory input, and it is somehow generating feelings of pain instead.
Phantom pain can be treated using dorsal root ganglion stimulation or deep brain stimulation.
Brachial plexus injury
The brachial plexus is a bundle of nerves in the neck that connect the spinal cord to nerves in the arm. The nerves in the brachial plexus carry signals from the brain to the muscles in the arm to control movement, and also carry sensory signals including touch and pain sensations in the other direction. The brachial plexus can be stretched or torn with a blow to the shoulder, and such injuries can lead to severe pain that is felt in the arm or hand. We see this most commonly in patients who have had motorcycle accidents.
If pain related to brachial plexus injury is unresponsive to medication it can be treated using spinal cord stimulation or deep brain stimulation.
Complex regional pain syndrome
CRPS is a poorly understood problem that has been given many different names in the past including "reflex sympathetic dystropy" (RSD), "Sudeck's atrophy", and "causalgia". Whilst the causes are uncertain, the clinical features are well known. The pain is usually in an extremity (arm or leg), is present constantly, and is typically burning, stabbing or throbbing in nature. Commonly it starts after an injury to the same area, which may have been relatively minor. There may be noticeable changes in the skin of the affected area including such things as swelling, redness, hotness (or occasionally coldness), excessive sweating and loss of skin hair. The area is often extremely painful when touched. Joint movements may be restricted and painful.
We have a range of techniques that may be useful for treating the pain of CRPS. These include spinal cord stimulation and dorsal root ganglion stimulation, and if these do not work there is the option of deep brain stimulation.
Post stroke pain
Central post stroke pain (CPSP) affects over 10% of stroke patients. It may feel icy, burning, or throbbing and commonly begins some months after the stroke, although it can sometimes occur immediately. It may respond to medications such as amitriptyline, gabapentin or pregabalin. Where pain is severe and medication is unsuccessful, deep brain stimulation may be considered.
We would emphasise that at present, this is one of the more challenging pain problems to treat with DBS. This is partly because the pain can extend over large body areas (for example sometimes it affects the whole of one side of the body including the arm, trunk, and leg) and the pain relieving effects of DBS are usually confined to smaller body regions than this. Another problem is that the stroke may have damaged the same parts of the brain that we would normally put an electrode into, so that the procedure is not possible. Each patient is different and we will discuss their symptoms with them to try to work out whether we can help.
Copyright OFN Wednesday, 11 February, 2015.