Deep brain stimulation
Deep brain stimulation (DBS) uses implanted wires to deliver small electrical pulses to specific parts of the brain. It is used in the treatment of movement disorders including Parkinson’s disease, dystonia, and tremor, as well as chronic severe pain. DBS leads are placed in precise brain locations that are chosen according to the type of symptoms to be addressed.
What is a deep brain stimulation system made up of?
The deep brain stimulation system consists of three components:
- depth leads that are inserted into the brain
- an implanted pulse generator (IPG) which is a small box that contains a battery and circuitry to produce the stimulus current pulses
- extension leads that connect the electrode leads to the IPG
 The tip of a depth lead showing its four contacts *
The tip of a depth lead showing its four contacts *The depth leads
These are thin cables containing several wires (usually four) which run to electrodes on the end of the lead that goes into the brain. Most commonly two leads are implanted, but sometimes only one, and very occasionally more than two may be needed.
The implanted pulse generator (IPG)
This is commonly referred to as the 'battery' but it also contains the circuitry that produces the small electrical current that is sent to the electrodes on the depth lead. It is a similar device to a heart pacemaker, and is usually implanted in a similar place, under the skin below the collar bone. You can usually see a bulge under the skin but most patients do not mind this. Some people prefer us to put it under the skin on the front of the abdomen (tummy) where it may be less obvious.
Two types of IPG are available:
- Rechargeable
- Non-rechargeable
For a description of the pros and cons of each type and how we choose between them, see our page on IPG types.
The extension leads
These are cables that connect the depth leads to the IPG. They are designed to be extremely flexible as they have to withstand being flexed back and forth as the neck moves.
How is a DBS system implanted?
Deep brain stimulation is performed in two stages. Stage 1 is an operation to very precisely place the depth leads into the exact location in the brain where they need to be to work well. Stage 2 is an operation to implant the extension leads and IPG. In some cases stage 2 is done on the same day right after stage 1. In other cases, when we are not sure how effective the system will be (this includes all pain cases), stage 2 is done several days later (typically 7 days later). During the gap between stage 1 and stage 2 the depth leads are tested on the ward to see if the stimulation is effective. If the results are good we proceed to stage 2 but if there is no beneficial effect we will simply remove the depth leads.
Stage 1
For many patients it is important that we can assess the response to stimulation during the operation, so that we can be sure that the leads are in the best possible position. For this reason stage 1 is commonly done under a local anaesthetic. However, patients with dystonia are usually treated under general anaesthesia because the benefits of DBS in dystonia usually take several months to appear and so testing during the operation is not useful.
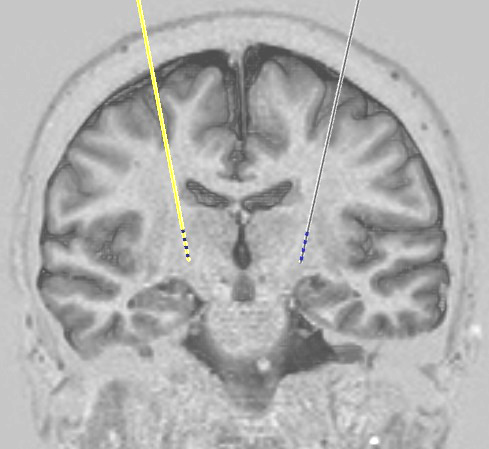
In order to place the brain electrodes very precisely, we used a technique called stereotaxy. This involves attaching a frame to the head which is used to guide everything to the right place. Once the frame is attached, a CT scan is done which allows us to see exactly where the brain is in relation to the frame. We use the MRI scan (done at an earlier date during the assessment process) together with this CT scan to produce coordinates for the electrode target position in the brain.
We then use the frame to drill a small hole in the skull (less than 3 millimetres wide) for each lead, and then to guide the lead into its position. When we get close to the target, we will start testing the effects of stimulating the lead. For example, we may test the effect on stiffness or tremor in PD, or we may ask if we are producing sensations in an area of the body where we are trying to treat pain. Once we are happy with the lead position, we secure the lead to the skull so that it does not move, and place the outside end of it under the scalp. If we are doing only stage 1 that day, we attach temporary extension wires which come out through the skin so that we can test the system using an external stimulator on the ward over the following few days.
We then do a second CT scan in order to check the position of the implanted lead(s).
Stage 2
This is done under general anaesthesia in all cases. Any temporary extension leads are removed. Then the implantable pulse generator (battery) is implanted, usually under the skin below the collar bone, and extension leads are run from it under the skin to reach the depth leads under the scalp. After connecting these parts together, we run electrical tests on the system to make sure all the components and connections are working properly.
After surgery
Following stage 2 patients are usually able to go home the next day. Instructions are provided about removal of stitches which can usually be done at the local GP surgery.
Switching the system on
Sometimes the system can be switched on before discharge from hospital, but in some situations we will leave it switched off for a few weeks. If a rechargeable battery has been implanted this may be because we need to give the wound time to heal before putting the recharger on top of it. For patients with PD we usually delay switch-on in order to allow time for the 'stun effect' to wear off. (Stun effect is a common situation where simply implanting the electrodes improves symptoms even before turning on the system. It is due to the brain area around the electrode tip being temporarily affected by the electrode insertion. The effect always wears off within a few weeks and symptoms return to baseline. If the stimulator is switched on while there is still stun effect the results can be unpredictable as the stun disappears.)
Any problems
If there are any problems with a system that we have implanted, please contact us. Patients are always given the contact details of one of our specialist nurses who should be the first port of call. They are available every weekday during working hours to talk to patients, relatives, or their general practitioners. In the event of an emergency occurring out of hours, advice should be sought from the on-call neurosurgical service at the John Radcliffe Hospital in Oxford.
The commonest complication with neuromodulation systems is infection which occurs in around 1 case in 20. The most likely time for this to appear is within the first few weeks to months after implantation of a new system or replacement of an old battery or pump. If there are any concerns about the appearance of a wound or any other symptom that might suggest infection, CALL US. If you are a patient then for this specific issue please call us rather than your GP. If you are a GP then please do not attempt to treat a possible wound infection with antibiotics but call us instead.
* Image courtesy of Medtronic
Copyright OFN Wednesday, 11 February, 2015.