Dorsal root ganglion stimulation
On each side of the spine along its length from the top of the neck to the bottom of the back, there are almost 30 "nerve roots" that connect the spinal cord to different parts of the arms, body, and legs. These nerve roots carry signals coming down from the brain that control your muscles, and they also carry sensory signals back in the other direction. The sensory signals convey the sense of touch but also include pain signals.
At the point where each nerve root enters the spine it has a bulge called the "dorsal root ganglion" or DRG. This is a key part of the pathways that carry the sensory and pain signals from the periphery to the spinal cord and onward to the brain. It has been found that electrical stimulation applied to the DRG can block the transmission of pain signals from the specific area of the body that the nerve root is running to.
What is a DRGS system made up of?
The system consists of two components:
- one or more electrodes that are inserted next to one or more DRGs
- an implantable pulse generator (IPG) which is a small box that contains a battery and circuitry to produce the stimulus current
The electrode
This is shaped like a straight wire with a curve on the tip to fit around the DRG. There are four electrical contacts near the tip to deliver the electrical pulses. The wire is passed into the spine through a large hollow needle. Up to four wires can be connected to one IPG so up to four DRGs can be stimulated, each with its own wire. However most patients require just one or two wires.
The implanted pulse generator
This is commonly referred to as the 'battery' but it also contains the circuitry that produces the small electrical current that is sent to the contacts on the electrode. If the electrode is being put in the lower back (e.g. for leg pain) the IPG is usually implanted under the skin of the abdomen (tummy). If the electrode is being put in the spine in the neck (e.g. for arm pain) the IPG may be implanted under the skin below the collar bone.
How is a DRG stimulator inserted?
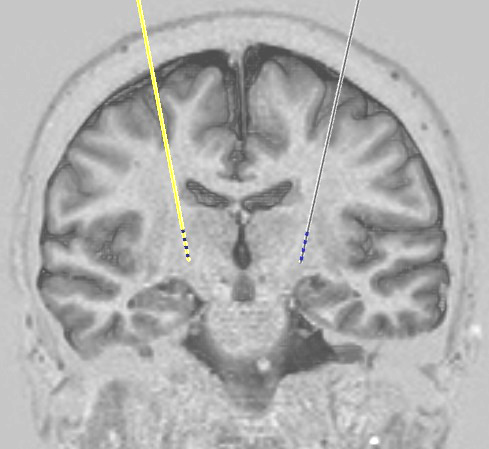
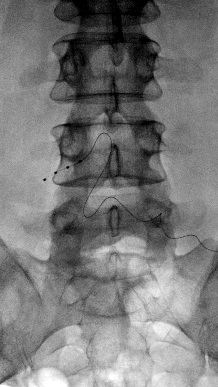 Xray showing DRG stimulator wire in place
Xray showing DRG stimulator wire in placeThe lead that carries stimulating pulses to the DRG is put in under local anaesthetic. When the skin has been numbed, a needle is passed into the space near the DRG and the lead is fed through it and guided into place using Xrays.
Because you are awake, we can test the effect of stimulation via the lead straight away. If the effects are good and clear cut, we can then complete the system by making a small incision nearby to allow placement of an implantable pulse generator under the skin and connecting the lead to it. If there is any uncertainty about how effective the test stimulation is, we will attach a temporary extension wire to the lead which is then brought out through the skin so that it can be tested for a few days using an external stimulator, before deciding whether the system is working well enough to complete it.
After surgery
In some cases DRGS can be done as day surgery. In other cases it is usually possible to go home the day after treatment. Instructions are provided for removal of stitches which can be done at the local GP practice.
Any problems
If there are any problems with a system that we have implanted, please contact us. Patients are always given the contact details of one of our specialist nurses who should be the first port of call. They are available every weekday during working hours to talk to patients, relatives, or their general practitioners. In the event of an emergency occurring out of hours, advice should be sought from the on-call neurosurgical service at the John Radcliffe Hospital in Oxford.
The commonest complication with neuromodulation systems is infection which occurs in around 1 case in 20. The most likely time for this to appear is within the first few weeks to months after implantation of a new system or replacement of an old battery or pump. If there are any concerns about the appearance of a wound or any other symptom that might suggest infection, CALL US. If you are a patient then for this specific issue please call us rather than your GP. If you are a GP then please do not attempt to treat a possible wound infection with antibiotics but call us instead.
Copyright OFN Wednesday, 10 August, 2016.